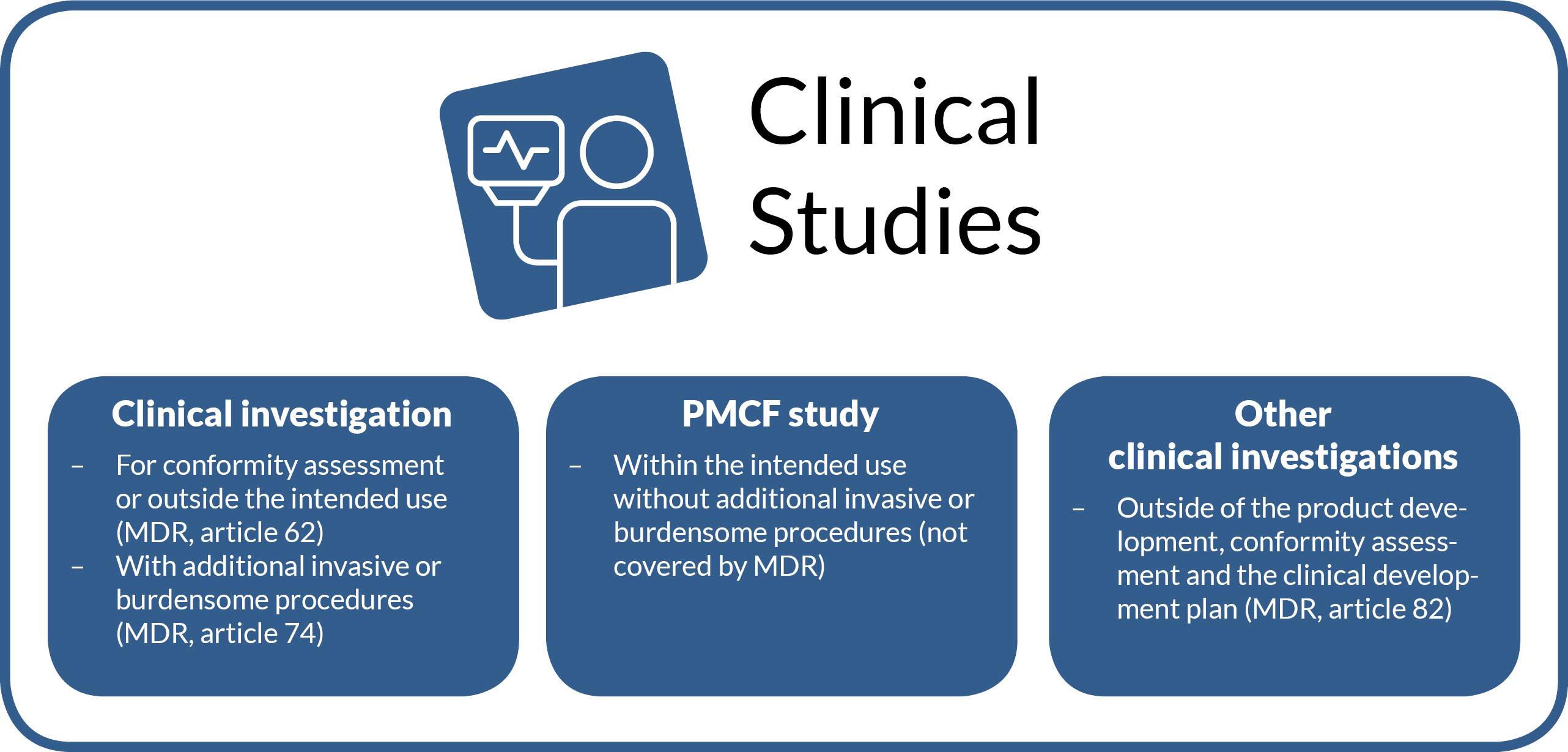
Types of clinical studies
There are different types of studies for medical devices. The choice depends on the regulatory status, the stage in the product’s lifecycle, and the type of product. In some cases, different approaches may be considered. Below, we describe the relevant types of studies.
Clinical investigation or clinical study?
First, it is important to clarify the terminology. The MDR and the MPDG use the term (other) clinical investigation. The MDR regulates clinical investigations before CE marking as well as after CE marking if the investigation involves additional invasive or burdensome procedures. However, the conduct of a clinical investigation with a CE-marked product within its intended purpose, without additional invasive or burdensome procedures, is not regulated by the MDR. Therefore, this type of clinical study is also not referred to as a “clinical investigation.” ISO 14155 treats the terms “clinical investigation,” “clinical trial,” and “clinical study” as equivalent.
Whether it is a clinical investigation before CE marking, after CE marking with additional invasive or burdensome procedures, a PMCF study, or another type of clinical investigation: for the sake of simplicity, we use the overarching term “clinical studies” when we are not explicitly referring to a clinical investigation or PMCF study. The decision tree from the Federal Ministry of Education and Research, published in the Medtec Online Guide, aids with classification and an overview. In the following, the individual types of studies are examined in more detail.
Clinical investigation to demonstrate conformity or with a CE-marked product outside the intended use (according to MDR, article 62)
A clinical investigation according to Article 62 of the MDR is a clinical investigation conducted to fulfill the general safety and performance requirements set out in Annex I of the MDR, before the medical device is lawfully placed on the market. The aim is to demonstrate that the medical device fulfills its intended purpose and the claimed benefits and is safe.
There are various ways to conduct a “pre-CE” clinical investigation. These include, for example, randomized controlled investigations or non-randomized investigations with or without blinding. In all cases, a favorable opinion from the ethics committee and approval from the federal competent authority are required before start of the clinical investigation. In addition, insurance for the patients is necessary, as the study procedure cannot be considered part of routine clinical care. Patients must give informed consent to participate in the clinical investigation and thus to the use of the investigational product (in the intervention group) or to randomization into a control group, if applicable. This type of clinical investigation is highly regulated and associated with various requirements for the investigation team (e.g. proof of qualifications and experience) and the sponsor (e.g., integration of sponsor activities into the quality management system, compliance with special reporting obligations, legal requirements, monitoring responsibilities).
Clinical investigation with CE-marked products according to MDR article 74 – with additional invasive or burdensome procedures
Article 74 of the MDR defines clinical investigations with medical devices that already bear a CE mark. These are clinical investigations conducted as part of post-market surveillance and involve additional burdensome or invasive procedures. According to ISO 14155 Annex I I.2.3, their purpose is to obtain further clinical data on the clinical performance, effectiveness, or safety of a medical device and to answer specific questions. The aim is to reassess the frequency of residual risks or side effects after the conformity assessment procedure or to identify unknown risks, as a larger number of patients is observed over a longer period.
If additional invasive or burdensome procedures are applied in the clinical investigation after CE marking compared to routine use, a favorable opinion from the ethics committee and notification to the federal competent authority are required before recruitment begins. Here too, informed consent from the patient is necessary, as these are study-specific procedures outside of routine clinical care. Depending on the nature of the additional procedures, it must also be decided whether to take out insurance.
PMCF studies according to (medical) professional regulations – with CE-marked products without additional invasive or burdensome procedures: data from routine clinical practice
Studies with medical devices that already bear the CE mark and are investigated within their intended purpose and without additional invasive or burdensome procedures are not covered by the MDR. These are considered biomedical research involving humans, in which the principal investigator must seek professional advice from the ethics committee in accordance with § 15 of the professional code for physicians. These studies are typically “observational studies,” in which data from routine clinical practice are collected and analyzed. A simple and effective way of data collection in this case is, for example, a registry or a user survey.
Since this type of study does not involve study procedures with the medical device under investigation, but only the analysis of data already contained in the medical record, only consent for data processing (in accordance with the General Data Protection Regulation, GDPR) and, if applicable, a waiver of confidentiality by the patient is required.
Digital health application (DiGA) – a special type of PMCF study: From conception to listing
Digital health applications, DiGA for short, are on everyone’s lips. Since 2019, the Digital Healthcare Act (DVG) has granted people with statutory health insurance the right to receive DiGAs prescribed by doctors or psychotherapists. If a relevant indication is present, the health insurance fund can also reimburse the use of a DiGA without a doctor’s prescription. As a purely German innovation with very specific requirements from the Federal Institute for Drugs and Medical Devices (BfArM), it is not trivial to complete all the necessary steps in a short time (keyword: “fast-track procedure”) and to achieve (permanent) reimbursement of the DiGA, or colloquially, the “app on prescription” through DiGA listing. The trial period for demonstrating the required positive healthcare effects is limited to one year, or two years in exceptional cases. With our experience, we can guide you safely through the requirements of the Digital Health Applications Ordinance (DiGAV) and the DiGA Guide—whether you are initially aiming for a provisional listing or the final one right away.
Has the BfArM set special requirements for your study? Together, we will find a satisfactory solution—from the pilot study to the RCT and all the way to listing. In this process, there are activities in addition to those in clinical investigations or “classic” PMCF studies that need to be implemented:
- Participation in consultation meetings with the BfArM, e.g. on strategies for demonstrating diagnoses, pilot study vs. main study, etc.
- Preparation of the evaluation concept
- Alternative methods of patient recruitment
Special challenges for this type of study arise from the nature of using an app as a medical device. We are happy to work with you to find new ways to recruit participants for the study and thus, also establish future distribution channels. To conduct studies as digitally as possible and, where possible, independently of study centers, your study can include not only electronic questionnaires but also online randomization and eConsent. Based on the study plan, we will decide together with you whether classic monitoring is possible for the study and will also justify these decisions to, for example, ethics committees or the BfArM.
Other clinical investigations (MDR, article 82)
Another special form of clinical investigation is the “other clinical investigation.” It is mentioned in Article 82 of the MDR, but is only explained in more detail in national legislation (here, MPDG §47). According to MPDG, Article 1, § 3, it is considered an “other clinical investigation” if it:
- is not part of a systematic and planned process for product development or product monitoring by a current or future manufacturer,
- is not conducted with the aim of demonstrating the conformity of a product with the requirements of Regulation (EU) 2017/745,
- serves to answer scientific or other questions and is conducted outside a clinical development plan according to Annex XIV Part A, Section 1, letter a of Regulation (EU) 2017/745.
Thus, “other clinical investigations” are irrelevant for the regulatory processes of manufacturers, but instead address the research needs of physicians as investigator-initiated trials (IITs). Depending on whether additional invasive or burdensome procedures are to be performed, either a favorable opinion from the ethics committee and notification to the federal competent authority is required, or professional consultation according to § 15 of the professional code for physicians is sufficient.

